What's the difference between a headache and a migraine?
We sat down with a Neurologist to understand the difference


Whether it’s the result of stress at work, eating too much sugar or your significant other packing the dishwasher incorrectly (again), most of us have experienced a headache at one time or another.
Oftentimes, these headaches can be treated by taking some pain relief, sipping water and having a rest.
However, there’s a big difference between a headache - even a very bad headache - and a migraine. With an estimated 4.9 million Aussies suffering from migraines, we sat down with Neurologist and Director of Migraine specialist, Dr Nicole Limberg, to understand the difference between the two.
Headache vs migraine
Headaches
Headaches are a common ailment that nearly all people experience at some stage in their life.
While headaches are unpleasant, especially when you experience them regularly over an extended period of time, they’re often situational and can be treated easily and quickly.
However, headaches can also be symptomatic of larger neurological health concerns, so it’s still important to see your GP if you are concerned.
Headaches can be brought on by anything that can cause our bodies stress, from emotions, foods, drinks and dehydration to smells and light. According to Headache Australia, headaches can be categorised into the following most common types:
Normal headaches – these include nerve stimulation, ice-cream, food reaction, MSG reaction, hangover, drug, fasting, rebound, exercise, coital, cough and mountain sickness headaches
Recurring headaches – tension or cluster headaches
Nerve headaches – compression of nerves directed to the head, face and neck causing pain and feelings of pressure
Muscle contraction headaches – which involve the tightening of muscles in the head
Medication misuse headaches – chronic headaches that come from misuse of medication
Head injury headaches – these come as a result of a blow to the head
While some people can be more prone to headaches than others, it’s a common ailment that almost everyone can relate to.
When it comes to migraines, however, it can be a very different experience.
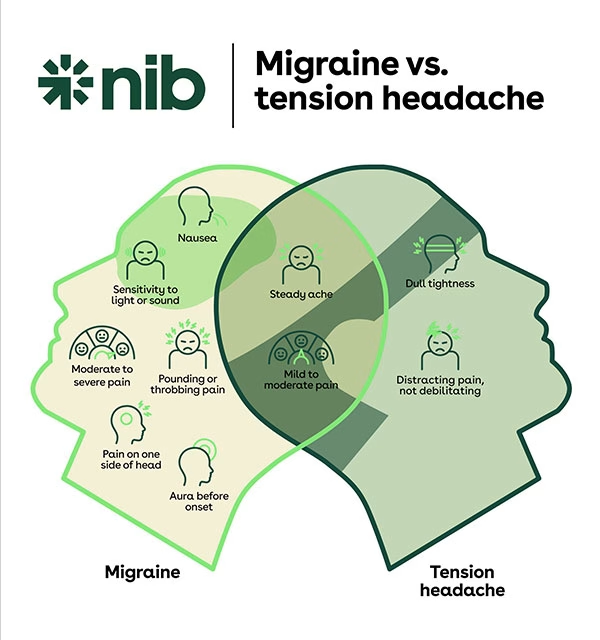
Migraines
A migraine is a neurological disorder that exists in various areas of the brain and can be both chronic (15 or more migraine days a month), or episodic (4-14 migraines per month).
Migraines are a more painful head and body pain than what a headache is. And, although the terminology is often interchanged, there are very big differences.
According to Nicole, migraines are far more debilitating and life altering than typical headaches, and can be classified as a disability in extreme cases.
“Migraine criteria is generally based on severity of pain - it’s a 6/10 at least - and understanding how much it is affecting someone’s ability to get through daily activity. Migraines are more disabling than people think; they affect sufferers’ ability to work, spend time with their family, and even just go outside or have the lights on,” Nicole explains.
Migraines can also last up to 72 hours, and when sufferers don’t have the migraine, they can get anxiety that one is coming and cause a headache in the spaces between migraines.
“Migraines can also last up to 72 hours, and when sufferers don’t have the migraine, they can get anxiety that one is coming and so causing a headache in the spaces between migraines. It’s a very serious affliction.”
Symptoms of migraines can be major sensitivity to sound and light, throbbing behind the eyes and around the head and face, nausea and vomiting, loss of appetite, dizziness and an inability to get through normal daily activity.
And, migraines can have far reaching consequences, from affecting relationships to quality of life and financial situations (Headache Australia estimates that the indirect and direct cost of migraine is about $35.7 billion each year).
Triggers for a migraine can be anything from light and sound to stress and environmental changes.
However, there are many successful treatments that can significantly improve the life of someone suffering from migraines. And it’s not simply a case of taking high dosage pain medication.
“We really look at the core triggers and the lifestyle factors that contribute to those triggers, rather than trying to Band-Aid the symptoms of a migraine with medication. Although we certainly assist with pain relief, it’s a greater priority to help people have a longer term solution,” explains Nicole.
“For example, if a patient’s trigger is a sensitivity to changes in their environment, we work with them to help improve this sensitivity and let the diminishment of migraines be symptomatic of that.”
Sometimes a combination of medication, acute therapy and preventative therapy is the best way to go.
“There are medication-based treatments that can also be helpful. Unfortunately, the prominence of migraines occur in people’s most productive time of life – career trajectory, growing families, etc. Sometimes a combination of medication, acute therapy and preventative therapy is the best way to go.”
So, what should you do if you’re suffering from migraines? The best way forward is to make an appointment with your GP for personalised advice and a professionally-directed treatment plan that will help you get your life back, as pain-free as possible. If you’re looking for a local GP, your first port of call should be nib's Find a Provider tool – you can use this tool to search for GPs in your area.
If you’re experiencing headaches from looking at a computer, smartphone or television screen, check out our article: Getting headaches? Here’s what you need to know about eye strain.
Getting headaches? Here’s what you need to know about eye strain
Here are some tips on relieving your eye strain symptom from an optometrist.
8 healthy habits to start in your 30s
It's the perfect time to lay the foundations of good health
8 ways to keep healthy in your 40s
Ditch the diet and start making some simple life changes
In partnership with
Dr Nicole Limberg
Dr Nicole Limberg is a Neurologist and the Director of Migraine Specialist in Brisbane. Dr Limberg has participated as an investigator in further research of chronic migraine therapy and data from her clinic has contributed to a retrospective chart review for the efficacy of injection therapy for the prophylaxis of chronic migraine in Australian clinical practice.