Bowel cancer: How to avoid Australia’s silent killer
In Australia, one in 19 people will develop bowel cancer


In Australia, one in 19 people will develop bowel cancer by the time they are 85 years old. Bowel cancer is estimated to be the fourth most commonly diagnosed cancer in Australia in 2021, and the second most common cause of cancer death.
So the likelihood that you, or someone you love will be affected is high.
The good news is that bowel cancer is highly treatable when discovered early. You can even take steps to help reduce your chances of getting it in the first place by making some simple lifestyle adjustments. Read on to find out how to reduce your risk of bowel cancer.
What is bowel cancer?
Bowel cancer, also known as colorectal cancer, develops in the large bowel (colon) or rectum. Most bowel cancers start as non-cancerous growths called polyps, which can turn into cancer over time (usually this takes years).
Often there are no symptoms in the early stages. When bowel tumour symptoms do develop they can include:
blood or mucus in stools
unexplained weight loss
extreme tiredness
a persistent change in bowel habits (going to the toilet more or less than usual, looser or narrower stools than usual
abdominal (tummy) pain
If you develop symptoms, don’t ignore them. Make an appointment to see your doctor as soon as possible.
How to avoid bowel cancer
While there are several risk factors for bowel cancer that you can’t change, such as your age and family history, there is still a lot you can do to reduce your risk. In fact, bowel cancer is one of the most preventable cancers. The two main things you can do include making lifestyle changes and participating in the National Bowel Cancer Screening Program.
Lifestyle changes to reduce your risk of bowel cancer
The following healthy lifestyle changes are things you can do to reduce your risk of developing the disease. A few small changes can make a big difference to your risk of getting bowel cancer.
1. Don’t smoke
Smoking increases your risk of bowel cancer along with many other cancers and serious illnesses. Stop smoking to reduce your risk and improve your health in general.
2. Watch your alcohol intake
Research has shown that having two or more alcoholic drinks a day significantly increases the risk of bowel cancer. So, keep your alcohol intake to fewer than two drinks per day.
3. Adjust your diet
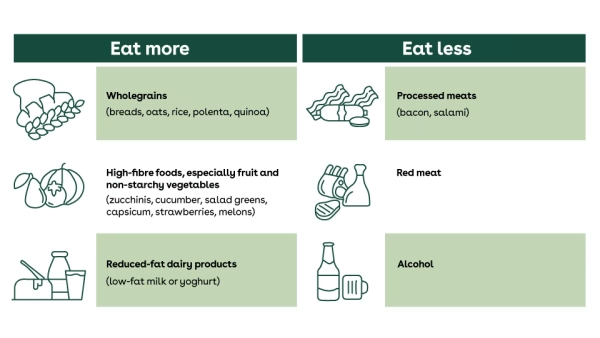
Recommendations on what to eat and what not to eat can sometimes be confusing. In general, wholegrains, high-fibre and dairy foods help reduce your risk of bowel cancer, while red and processed meats can increase your risk.
Processed meats are meats that have been smoked, cured, salted or processed in some way. Think salami, hot dogs, ham, bacon, canned meat, jerky and corned beef. Try to avoid these as much as possible.
The Cancer Council Australia recommends eating a maximum of 455 grams of lean, cooked red meat per week (like beef, veal, pork, lamb, mutton, venison and goat). Also avoid burning meat when cooking on the BBQ, as burnt or charred meat can also contribute to an increased risk of bowel cancer.
While it’s still unproven, there is some evidence to show that fish and foods containing vitamin C might be protective against bowel cancer.
4. Get moving
Being physically active reduces your risk of bowel cancer. Aim for at least 30 minutes of activity that’s intense enough to raise your heart rate every day. As you get fitter, try for 60 minutes a day or increase the intensity - and limit sedentary activities such as watching TV.
5. Stay trim
Being overweight can increase your risk of bowel cancer, so make every effort to maintain a healthy weight or lose weight if you are overweight.
If you need some help losing weight, nib offers Healthy Weight for Life Essentials, available to eligible nib members at no additional cost1 who’ve been diagnosed with a chronic disease and have a BMI of 28 or over. Head to our Health Management Programs page for more information.
Bowel cancer screening
If you’re aged 50 or older, the National Bowel Cancer Screening Program should be on your radar. As part of the program, all Australians are sent a free test kit in the mail every two years from the ages of 50 to 74.
Screening aims to find bowel cancers early, before they’ve grown large enough to cause symptoms. When you detect bowel cancer at an early stage, cure is much more likely. The bowel cancer screening program has been shown to reduce deaths from bowel cancer and the program could save up to 500 lives each year.
Because the risk of bowel cancer starts to increase sharply from the age of 50, screening is recommended from this age for most people.
Who should do the test?
Because the risk of bowel cancer starts to increase sharply from the age of 50, screening is recommended from this age for most people.
People who have a higher than average risk due to their family history or other conditions (such as inflammatory bowel disease) may be advised to have tests from a younger age.
And anyone who has symptoms should see their GP. The test used in the screening program is not recommended for people experiencing symptoms.
What’s involved?
The test used in the National Bowel Cancer Screening Program is called a faecal immunochemical test (FIT), which can detect tiny amounts of blood in your stool that you can’t see with the naked eye.
You do the test at home and then send the test card in a postage paid envelope to a lab for testing. The results will be sent to you and your GP if you ask for this to occur. Depending on the results, further tests may be recommended.
Don’t die of embarrassment
Most of us feel slightly uncomfortable at the thought of doing this type of test. But it’s really simple and not actually that embarrassing. And it could save your life. Surely that’s worth putting up with the ‘ick’ factor?
What does a positive test mean?
A positive test means that some blood has been detected. But the test can’t tell what is causing the blood in your stool. Bowel inflammation, haemorrhoids, polyps and early bowel cancer can all cause bleeding. Most people with a positive test don’t have bowel cancer.
If your results are positive for blood, your doctor will recommend that you have another test - usually a colonoscopy - to look inside your bowel to see what could be causing the bleeding. If polyps are found during the colonoscopy, they may be able to remove them during the procedure.
What to do if you get a negative result
If your screening test result comes back negative, it means that no blood was found. In most cases you don’t need to do anything until the next test arrives in the post in two years’ time.
But a negative result doesn’t guarantee that you don’t have or won’t get bowel cancer. So if you do develop symptoms - especially bleeding - at any time, see your doctor straight away. The bowel cancer screening test is not a replacement for a regular check-up with your doctor.
Keen for more information on how to reduce your risk of bowel cancer? Check out our article Why fibre should be on your shopping list.
1Available to eligible nib members who’ve held Hospital Cover for 12 months and served their relevant waiting periods. Additional criteria vary according to each program.
Getting headaches? Here’s what you need to know about eye strain
Here are some tips on relieving your eye strain symptom from an optometrist.
8 healthy habits to start in your 30s
It's the perfect time to lay the foundations of good health
8 ways to keep healthy in your 40s
Ditch the diet and start making some simple life changes